
Understanding Breast Cancer Stages (Updated 2021)
Once you are diagnosed with breast cancer, it is crucial to know what stage it is in. In doing so, you will have an informed decision on the next steps you need to take. Your doctor will guide you throughout the diagnosis and provide you the information that you need, however, even before being diagnosed with the disease, or if you know someone who’s been diagnosed with breast cancer, it would be helpful to familiarize yourself with the breast cancer stages to have a better understanding of how it can progress from Stage 0 to IV.
Doctors have several ways of determining what stage of cancer you have. Initial symptoms of the disease can be pointed out through medical tests like physical exams, biopsies, X-rays, bone scans, and blood tests. Furthermore, a pathologist gets a tissue sample from the breast tissue or lymph node and exam it for diagnosis through a microscope.
Based on the results of the tests, the doctor will be able to name the stage of breast cancer. The stages are numbered 0 to, Roman numerals, I to IV, where a higher number means a more advanced cancer. The number is followed by a letter (A, B, or C) to further explain the state of the disease.
Breast cancer stages
Stage 0
Stage 0 is the earliest detection of breast cancer, where the cancer cells have stayed in the ducts or milk glands and not yet developed. It is also called carcinoma in situ (in situ, meaning “in the original place”). However, this stage is commonly harder to detect because there may not be a lump during self-examination or no other symptoms showing. It is most often found by accident during a breast biopsy for other reasons, such as to investigate an unrelated breast lump. Still, self-exams and routine screenings are important for early diagnosis.
Stage 0 breast cancer can be classified into two types:
Ductal carcinoma in situ (DCIS)
This type occurs when the breast cancer cells develop in the breast ducts. It can become invasive and early diagnosis and treatment are needed.
Lobular carcinoma in situ (LCIS)
This type occurs when the abnormal cells develop in the lobules. It is not cancerous and rarely becomes invasive. However, if you are diagnosed with LCIS, there is a higher risk for you to develop breast cancer in the future.
Stage I
Stage I is the earliest stage of invasive breast cancer, where the cancer cells have spread to the surrounding breast tissues. This stage is still a little difficult to detect because of the small size of the tumor.
It is further divided into two subcategories:
Stage IA
The tumor is around 2 cm and has not spread beyond the breast, where no lymph nodes are affected.
Stage IB
This stage can manifest in two ways:
- No tumor is located in the breast, but there are small groups of cancer cells- larger than 0.2 mm but not larger than 2 mm- in the lymph nodes.
- There is a tumor located in the breast, no larger than 2cm, and there are small groups of cancer cells- larger than 0.2 mm but not larger than 2 mm- in the lymph nodes.
Stage II
During Stage II, the tumor has grown in size or the cancer cells have spread to the surrounding breast tissues or lymph nodes, but not to distant parts of the body. At worse, it can be both. Here, a tumor is more prominent during a self-exam when you feel a hard lump within the breast.
Just like Stage I, it is further divided into two subcategories:
Stage IIA
It is considered Stage IIA if either of these cases happens:
- There is no tumor in the breast, but cancer cells (larger than 2mm) are located in 1 to 3 axillary lymph nodes under the arm or near the breast bone.
- The tumor is2cm and cancer has spread to the axillary lymph nodes.
- The tumor is larger than 2cm but smaller than 5cm, and cancer cells have not spread to the axillary lymph nodes.
Stage IIB
It is labeled as Stage IIB if either of the following happens:
- The tumor is larger than 2cm but smaller than 5cm, and there are small groups of cancer cells- larger than 0.2 mm but not larger than 2 mm- in the lymph nodes.
- The tumor is between 2cm to 5cm and cancer cells are located in 1 to 3 axillary lymph nodes under the arm or near the breast bone.
- The tumor is larger than 5cm but cancer cells have not spread to the axillary lymph nodes.
Stage III
Stage III is known as locally advanced breast cancer, the cancer is extensive in the underarm lymph nodes or has spread to other lymph nodes or tissues near the breast. At this stage, the cancer cells have not spread to bones and organs, but they are present in several axillary (underarm) lymph nodes. The tumor may also be quite large at this stage, possibly extending to the chest wall or the skin of the breast, making it harder for treatment.
Unlike the previous stages, it is further divided into three subcategories:
Stage IIIA
It is classified as Stage IIIA under either of the following conditions:
- There is no tumor in the breast, or the tumor may be any size, and cancer cells are found in 4 to 9 axillary lymph nodes under the arm or near the breast bone.
- The tumor is larger than 5 cm and small groups of breast cancer cells- larger than 0.2 mm but not larger than 2 mm- are in the lymph nodes.
- The tumor is larger than 5cm and the breast cancer cells spread to 1 to 3 axillary lymph nodes under the arm or near the breast bone.
Stage IIIB
Stage IIIB manifests in either of the following conditions:
- The tumor may be any size and the cancer cells have spread to the chest wall and/or skin of the breast, which leads to swelling or ulcer.
- Cancer has spread to up to 9 axillary lymph nodes under the arm.
- Cancer cells have spread to lymph nodes near the breastbone.
Stage IIIC
It is considered Stage IIIC if any of the following happens:
- There are no signs of cancer in the breast or if a tumor is located, it may be any size. Cancer cells also have spread to the chest wall and/or the skin of the breast.
- Cancer has affected 10 or more axillary lymph nodes.
- Cancer cells have spread to lymph nodes above or below the collarbone.
- Cancer has affected the axillary lymph nodes under the arm or near the breast bone.
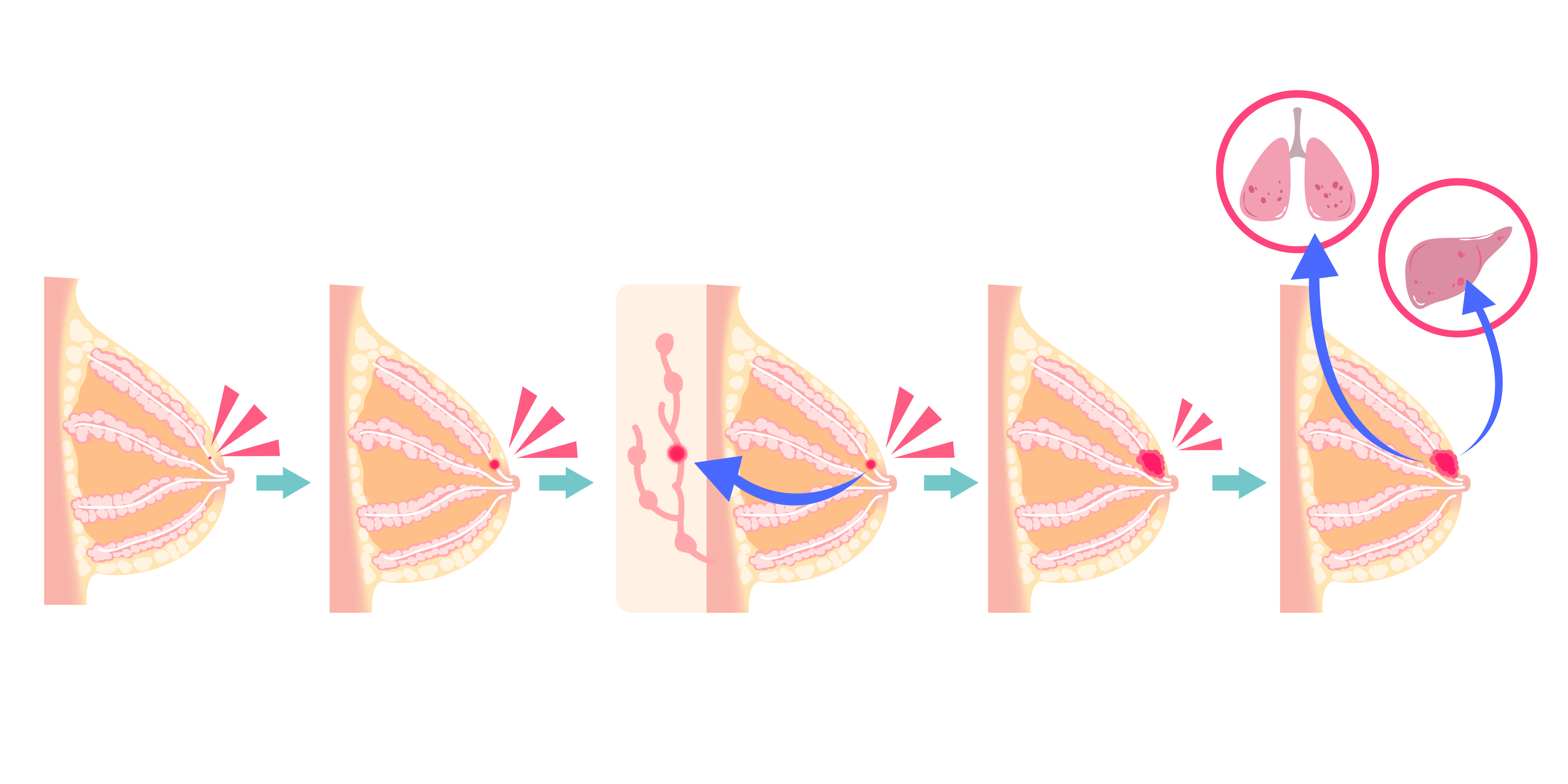
Stage IV
Stage IV is the most complicated stage of breast cancer. It is known as metastatic breast cancer, meaning it has spread through the body from the area it was first found. Here, cancer cells have affected the breast, lymph nodes, and other organs in the body, such as the lungs, liver, bones, and brain.
At this stage, and other stages of breast cancer, the doctor usually uses the TNM Staging System to elaborate on the extent of the condition.
TNM Staging System
The TNM Staging System is a common tool used by professionals to describe the stages of breast cancer. It has three categories: Tumor (T), Node (N), and Metastasis (M).
Tumor (T)
This refers to the size of the lump or tumor. It is followed by a numerical value suggesting the size of the tumor. A higher number means a bigger or wider lump. The stage of cancer can be classified as either of the following:
- TX: The tumor cannot be evaluated.
- T0: There are no signs of cancer in the breast.
- Tis: The cancer is “in situ”, or the tumor has not started growing in healthy breast tissues.
- T1: The tumor is 20mm or smaller.
- T1mi: a tumor that is 1 mm or smaller.
- T1a: a tumor that is larger than 1 mm but smaller than 5mm.
- T1b: a tumor that is larger than 5 mm but smaller than 10mm.
- T1c: a tumor that is larger than 10 mm but smaller than 20mm.
- T2: The tumor is larger than 20mm but smaller than 50mm.
- T3: The tumor is larger than 50mm.
- T4: The tumor has grown into the chest wall and/or skin, or it has become inflammatory breast cancer.
Node (N)
This category looks if the cancer cells have reached the nearby lymph nodes and, if so, how many has it affected. It can be classified as any of these cases:
- NX: The lymph nodes cannot be evaluated.
- N0: There are no signs of cancer in the lymph nodes or cancer cells smaller than 02.mm are in the lymph nodes.
- N1: Cancer cells have spread to 1 to 3 axillary lymph nodes and/or the internal mammary lymph nodes. If the cancer in the lymph node is larger than 0.2 mm but smaller than 2 mm, it is called “micrometastatic” (N1mi).
- N2: Cancer cells have spread to 4 to 9 axillary lymph nodes, or it has spread to the internal mammary lymph nodes, but not in the axillary lymph nodes.
- N3: Cancer cells have spread to more than 10 axillary lymph nodes, or it has spread to the internal mammary and supraclavicular lymph nodes.
Metastasis (M)
This category identifies if there are signs of cancer in other areas of the body, spreading beyond the breast and lymph nodes. It can be either of the following:
- MX: Distant spreading cannot be evaluated.
- M0: Cancer has not affected other parts of the body.
- M0 (i+): There are no clinical or radiographic signs of distant spreading. However, Microscopic evidence of cancer cells, no larger than 0.2mm, is located in the blood, bone marrow, or lymph nodes.
- M1: Cancer cells are forming in other organs of the body.
Next Step After Being Diagnosed
More than the illness itself. It is also a matter of getting a cure that needs to be understood. There are different ways to remove the cancer cells that have formed on the breast or reconstruct the breast. These are Mastectomy, Breast Reconstruction, and Prophylactic Mastectomy.
- Mastectomy
- A mastectomy is done mostly on patients who have a high risk of having breast cancer. Breast tissues such as the lymph nodes are removed or the entire breast for those who are looking forward to completing breast cancer-free breasts.
- A mastectomy is done mostly on patients who have a high risk of having breast cancer. Breast tissues such as the lymph nodes are removed or the entire breast for those who are looking forward to completing breast cancer-free breasts.
- Types of Mastectomy
- Total Mastectomy
- This procedure removes every part of the breast including the nipple, the areola, and the overlying skin.
- Modified Radical Mastectomy
- The modified radical mastectomy is almost the same as the total mastectomy, the only difference is. It also removes the lymph nodes. In which these lymph nodes can become a trigger to spread cancer. And so for others, they opt to have it removed as well.
- The modified radical mastectomy is almost the same as the total mastectomy, the only difference is. It also removes the lymph nodes. In which these lymph nodes can become a trigger to spread cancer. And so for others, they opt to have it removed as well.
- Radical Mastectomy
- Compared to total mastectomy and modified radical mastectomy, radical mastectomy includes the chest muscles under the breast. And sometimes, lymph nodes under the arm.
- Compared to total mastectomy and modified radical mastectomy, radical mastectomy includes the chest muscles under the breast. And sometimes, lymph nodes under the arm.
- Skin-sparing Mastectomy
- This removes the entire breast including the breast tissue, nipple, and areola but it keeps most of the skin over the breast. This procedure is commonly done after the mastectomy. With that being said, It may not be suitable for tumors that are large or that are near the skin surface.
- This removes the entire breast including the breast tissue, nipple, and areola but it keeps most of the skin over the breast. This procedure is commonly done after the mastectomy. With that being said, It may not be suitable for tumors that are large or that are near the skin surface.
- Nipple-sparing Mastectomy
- This method is not commonly advised. The breast tissue, including the nipple and areola, is removed. Here in this method, the skin of the nipple and areola are kept. They cut the tissues under and around the nipple and areola. A pathologist will be checking the breast to know whether there are remaining cancer cells close to the nipple and areola.
- This method is not commonly advised. The breast tissue, including the nipple and areola, is removed. Here in this method, the skin of the nipple and areola are kept. They cut the tissues under and around the nipple and areola. A pathologist will be checking the breast to know whether there are remaining cancer cells close to the nipple and areola.
- Total Mastectomy
- Breast Reconstruction
- Usually, breast reconstruction is done after mastectomy. This is to rebuild or reconstruct the breast after having it removed. In some cases when the nipples are also absent from the mastectomy, this also will be part of the surgery. Doctors may take tissues from the skin in softer parts of the body such as the inner thigh to rebuild the nipple, and also the areola. However, in some cases, this does not assure the sensation of having natural nipples.
- This procedure also uses breast implants to replace the fullness of the breast.
- Usually, breast reconstruction is done after mastectomy. This is to rebuild or reconstruct the breast after having it removed. In some cases when the nipples are also absent from the mastectomy, this also will be part of the surgery. Doctors may take tissues from the skin in softer parts of the body such as the inner thigh to rebuild the nipple, and also the areola. However, in some cases, this does not assure the sensation of having natural nipples.
- Prophylactic Mastectomy
- Prophylactic mastectomy is a procedure done to remove one or both breasts to minimize the risk of developing breast cancer.
- Types of Prophylactic Mastectomy
- Bilateral Prophylactic Mastectomy
- Bilateral prophylactic mastectomy is the removal of both breasts to prevent the risk of having breast cancer. It is said that a Bilateral Prophylactic Mastectomy has a percentage of 90% in reducing the risk. Even so, this does not completely remove the chance of having breast cancer because it cannot remove all of the breast tissues. Giving it a slight chance of still having breast cancer.
- Bilateral prophylactic mastectomy is the removal of both breasts to prevent the risk of having breast cancer. It is said that a Bilateral Prophylactic Mastectomy has a percentage of 90% in reducing the risk. Even so, this does not completely remove the chance of having breast cancer because it cannot remove all of the breast tissues. Giving it a slight chance of still having breast cancer.
- Contralateral Prophylactic Mastectomy
- On the other hand, this procedure is about removing the healthy breast of a woman who has been diagnosed with breast cancer.
- On the other hand, this procedure is about removing the healthy breast of a woman who has been diagnosed with breast cancer.
- Bilateral Prophylactic Mastectomy
- Prophylactic mastectomy is a procedure done to remove one or both breasts to minimize the risk of developing breast cancer.
What to Consider for Breast Reconstruction?
- Prepare yourself both physically and mentally.
- Going under another operation after a Mastectomy may become overwhelming. Nevertheless, for some, this is what they might need to gain back confidence. And it is not wrong if you wish to have one. However, it is important that you make sure to discuss the procedure with a surgeon qualified for breast reconstruction. You may want to hear the process of the surgery to make sure that it will meet your expectations.
- Going under another operation after a Mastectomy may become overwhelming. Nevertheless, for some, this is what they might need to gain back confidence. And it is not wrong if you wish to have one. However, it is important that you make sure to discuss the procedure with a surgeon qualified for breast reconstruction. You may want to hear the process of the surgery to make sure that it will meet your expectations.
- Finding a qualified Plastic Surgeon
- A plastic surgeon is often advised by your general surgeon after conducting a mastectomy or your doctor after being diagnosed with breast cancer. For some who seek reconstruction after the mastectomy, they find their plastic surgeon. And it is very important to understand which doctor best fits the procedure.
- The internet may come up with many results, but make sure not to get confused with the different titles of a surgeon. Make sure you look for a plastic surgeon who is practiced and licensed to operate breast reconstruction. Because some surgeons only do breast implants or fixing tissue flaps. Do not hesitate to ask your surgeon if he can do the procedure. If you think you are not convinced with the surgeon, you are free to make a consultation with other surgeons that may best suit your needs.
- A plastic surgeon is often advised by your general surgeon after conducting a mastectomy or your doctor after being diagnosed with breast cancer. For some who seek reconstruction after the mastectomy, they find their plastic surgeon. And it is very important to understand which doctor best fits the procedure.
- Look For Quality Implants
- Both saline and silicone implants are safe to use for breast reconstruction. Saline Implants are implants filled with salt water while Silicone implants are filled with silicone gel and tend to give a more natural feel and look, similar to natural breasts.
- Each implant has a different size and texture. Either smooth or textured implants. However, as of today, it is more often to use silicone-gel implants than saline because it has less possibility of having ruptures.
- It is important to know which implant is best to use when going for breast reconstruction because these will technically become your new set of breasts. Make sure that the implants are safe, clean, clinically approved. Also, are safe from possible complications that can harm you more than save you.
- Both saline and silicone implants are safe to use for breast reconstruction. Saline Implants are implants filled with salt water while Silicone implants are filled with silicone gel and tend to give a more natural feel and look, similar to natural breasts.
MOTIVA Implants®
When it comes to implants, it is always best to choose a product that meets all your needs. Including, safety, security, and an implant that has a size that will be perfect for your body frame.
What’s good about MOTIVA Implants® is, it has properties that will meet the expectations of patients who want a result that is close to natural breast. With Motiva Ergonomix™ it is possible to build new breasts without making the patient feel that they are wearing implants. This can be one of the best choices for breast cancer patients who seek breast reconstruction. to boost their confidence and at the same time be comfortable. Being provided with a more natural look and feel, regardless of the position, mirroring the movement of natural breast tissue by gravity. The patented technology of Ergonomix® allows Minimal Scar Breast Augmentation without impairing the mechanical properties of the implants under stressful circumstances.
Understanding the different stages of breast cancer can help you gain more knowledge on how to prevent and cure future risks and serious possibilities. But if ever you do feel that you are on the verge of having the disease, do not overthink the following situations you may face ahead. Consult your doctor when needed. And to get more professional information on how to deal with breast cancer.
If you may eventually conclude to have mastectomy and breast reconstruction, be open to what your doctor will advise. Make sure to be in-depth with the details in order for you to prepare yourself both physically and mentally.
